"Airway Dentistry" - let's unpack the latest trend in the dental profession.
“In recent years, parts of airway dentistry have pivoted into unsubstantiated marketing claims; frenectomy has been pitched as a fix for Obstructive Sleep Apnea (OSA), Attention Deficit Hyperactivity Disorder (ADHD), anxiety, and behavioral issues; MARPE/SARPE expansion has been sold as a definitive airway fix for adults.".
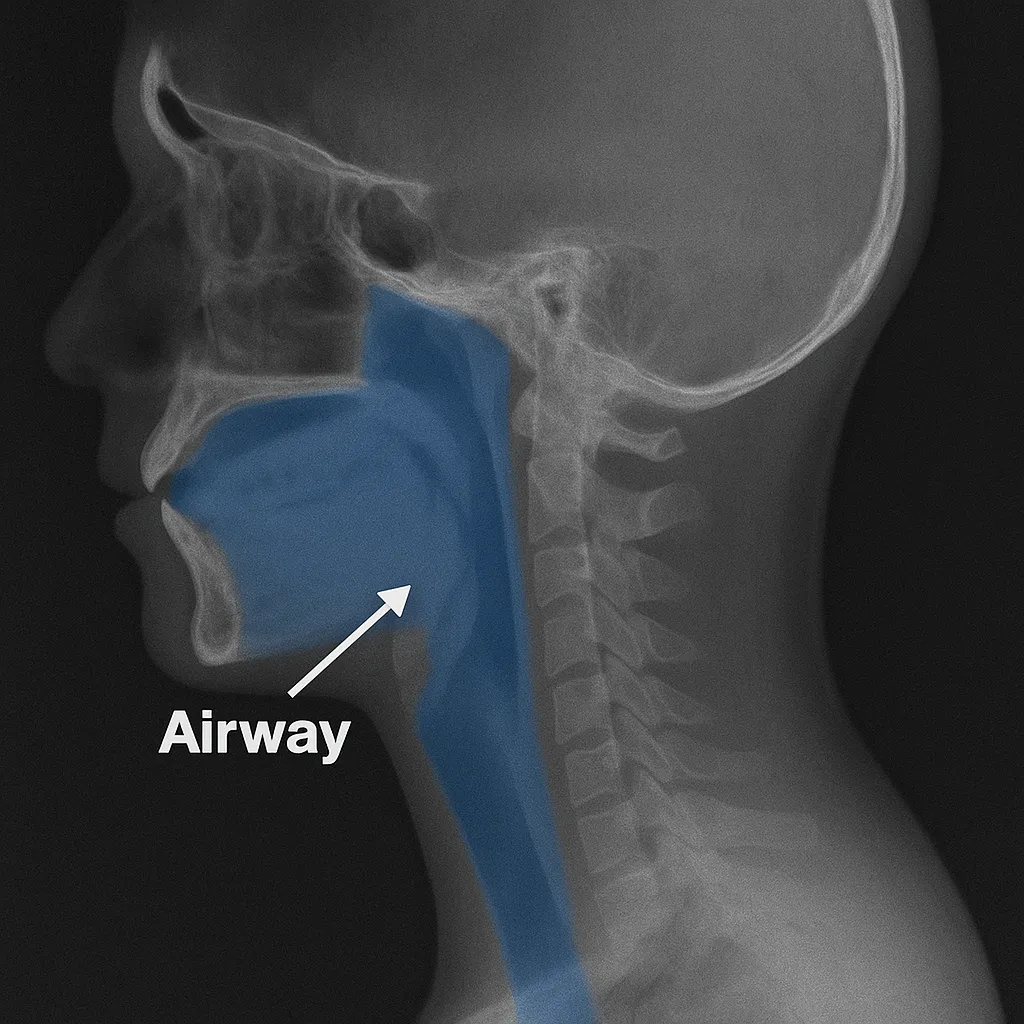
Dentists have always been among the early clinicians to identify risk factors for obstructive sleep apnea, such as a narrow palate, an underdeveloped lower jaw (retrognathic mandible), and signs of mouth breathing; in many ways, dentists have always practiced “airway” dentistry since its inception. But this blog discusses how a seemingly routine, benign concept can acquire a life of its own with bizarre theories and expensive treatments sold under “airway” dentistry.
Let’s start with what I agree on with Airway Dentistry providers : Oral appliances for Obstructive sleep apnea, which I’ve blogged about before. Oral appliance therapy, which advances the lower jaw forward, is a well-supported intervention for mild to moderate OSA [1]; randomized and guideline data confirm its safety and efficacy when used appropriately [2]; it’s one part of “airway dentistry” I wholeheartedly support [3].
And here is where I challenge current "Airway" dentistry recommendations.
In recent years, parts of airway dentistry have pivoted into unsubstantiated marketing claims; frenectomy has been pitched as a fix for OSA, Attention Deficit Hyperactivity Disorder (ADHD), anxiety, and behavioral issues; MARPE/SARPE expansion has been sold as a definitive airway fix for adults. I’ve already blogged here about why both procedures are not good recommendations in the management of sleep apnea, TMD, and headache disorders.
Cone-Beam Computed Tomogram dental images (CBCTs), can record airway volume changes and it was initially thought expanded airway volume could decrease snoring and sleep apnea. But future research established established that airway changes seen in CBCT from expansion of the palate do not correlate with improved breathing or decreased sleep apnea [4][5]. Anatomic changes from expansion do not necessarily lead to functional changes; they don’t guarantee better sleep or improved breathing. Adult palatal expansion rarely yields durable, clinically meaningful improvements in validated sleep outcomes [4][5].
Similarly, frenectomy will not address neurological issues; claims of curing Attention Deficit Hyperactivity Disorder (ADHD) with a soft-tissue snip are so absurd they don’t merit scientific airtime. Dentistry should not pretend that a frenectomy reverses a complex neurodevelopmental disorder.
Many airway dentists have begun advocating early interventions in children—especially palate expansion to “prevent” future sleep apnea and TMD. Phase 1 orthodontics at a young age to create space for erupting teeth is a mainstream orthodontic concept and my own child has had it to create space in a crowded jaw. But even orthodontists themselves do not claim that expansion or frenectomy prevents future sleep apnea or future jaw pain. Obstructive sleep apnea is far more complex than jaw space alone; temporomandibular joint dysfunction reflects biopsychosocial interactions rather than simple anatomic deficits [6][7][8]. Palate expansion may confer orthodontic benefits, but there’s no credible proof it prevents future airway or TMJ disorders.
There is no recognized dental specialty called “airway” dentistry; the Wisconsin Dentistry Examining Board explicitly prohibits dentists from advertising themselves as “specialists” unless they’ve completed a CODA-approved residency program in an ADA-recognized specialty. Advertising a non-recognized specialty, such as “airway specialist”, is considered unprofessional conduct under Wisconsin Administrative Code DE 6 [9].
The American Association of Orthodontists has also taken a clear position: orthodontic treatment, including palate expansion, should not be represented as a treatment for OSA or airway disorders in the absence of sufficient evidence; multidisciplinary medical evaluation remains the standard of care [10]. In short: the people who actually own the orthodontic specialty have already said what some “airway” gurus refuse to admit.
This is one more blog where I ask the readers: maybe I should cave in, join the groups peddling expensive treatments for sleep apnea, and finally upgrade my 2022 Toyota RAV4 Hybrid to something fancier.
REFERENCES
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, Chervin RD. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015;11(7):773–827. doi:10.5664/jcsm.4858.
Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F, Kushida CA, Cistulli PA. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014;10(2):215–227. doi:10.5664/jcsm.3460.
Lim J, Lasserson TJ, Fleetham J, Wright J. Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;1:CD004435. doi:10.1002/14651858.CD004435.pub3.
Papageorgiou SN, Jambi S, Patcas R, et al. Effects of rapid maxillary expansion on the upper airway: a systematic review and meta-analysis with meta-regression. Eur J Orthod. 2024;47(2):cjaf012. doi:10.1093/ejo/cjaf012.
Jafari A, Rinaldi V, Cerruto C, et al. CBCT-based upper airway volume changes do not predict functional breathing outcomes: a systematic review. Sleep Breath. 2024;28:981–993. doi:10.1007/s11325-023-02972-7.
Baccetti T, Franchi L, McNamara JA Jr. Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71(5):343–350. doi:10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2.
Papageorgiou SN, Jambi S, Patcas R, et al. Effects of rapid maxillary expansion on the upper airway: a systematic review and meta-analysis with meta-regression. Eur J Orthod. 2024;47(2):cjaf012. doi:10.1093/ejo/cjaf012.
Ohrbach R, Dworkin SF. The evolution of TMD diagnosis: past, present, future. J Dent Res. 2016;95(10):1093–1101. doi:10.1177/0022034516653922.
Wisconsin Administrative Code, Dentistry Examining Board Chapter DE 6 — Unprofessional Advertising. (Wis. Admin. Code DE 6.02(4)(c)).
American Association of Orthodontists. Statement on Obstructive Sleep Apnea and Orthodontics. AAO White Paper. 2019
..
