Burning Mouth Syndrome
Let us help you find relief, regain comfort, and live well.
At Oral Medicine of Wisconsin, we understand that oral comfort is essential to your overall health, well-being, and quality of life. For patients living with burning mouth syndrome—a persistent, often painful condition marked by a burning sensation in the mouth—specialized care can provide meaningful, lasting relief.
WHAT IS BURNING MOUTH SYNDROME?
Burning Mouth Syndrome (BMS) is a chronic condition characterized by a burning, scalding, or tingling sensation in the mouth, most commonly affecting the tongue, lips, palate, or entire oral cavity. Despite its intensity, there are often no visible signs of irritation or inflammation inside the mouth.
Do You Have BMS?
Burning Mouth Syndrome (BMS) is a complex condition characterized by a persistent burning, tingling, or numb sensation in the tongue or other areas of the mouth. Many people with BMS also notice a dry mouth or increased thirst, and some experience an altered or metallic taste. It’s common to feel as though the mouth is sore or raw, even though there may be no visible signs during an exam. For some, symptoms may fluctuate or come and go, but they often become more noticeable as the day progresses.
BMS can affect anyone, but it is most frequently seen in women—particularly those in midlife or postmenopausal stages. However, both men and women of any age may develop this condition.
The causes of BMS can be difficult to pinpoint. In some cases, it is considered primary (idiopathic), likely related to nerve dysfunction that affects taste and pain pathways. Secondary BMS may be associated with underlying factors such as nutritional deficiencies (like vitamin B12, iron, or folate), oral infections, dry mouth, hormonal changes, gastrointestinal reflux, or allergic reactions. Psychological factors—including anxiety, stress, or depression—can also influence the severity of symptoms.

Diagnosis
Diagnosing Burning Mouth Syndrome (BMS) is often a process of exclusion, as there is no single test that can confirm the condition. Your dental specialist will take a thorough approach to rule out other possible causes of your symptoms. This may include:
A detailed review of your medical and dental history
Blood tests to check for vitamin deficiencies or systemic health issues
Oral swabs or biopsies to rule out infections or other oral diseases
Salivary flow tests to assess for dry mouth
Allergy testing to identify potential sensitivities
These steps help ensure that any underlying issues are identified and addressed as part of your care.

Treatment
Because BMS often results from a combination of factors, treatment is highly individualized. Your care plan may involve:
Managing any underlying medical conditions contributing to your symptoms
Using saliva substitutes or medications to relieve dry mouth
Supplementing with vitamins and minerals if deficiencies are found
Prescribing medications such as antidepressants, anticonvulsants, or topical agents to target nerve-related pain
Recommending cognitive-behavioral therapy to help manage stress or anxiety that may worsen symptoms
Living with BMS
Though BMS can be frustrating and difficult to treat, many patients experience improvement through a comprehensive, multidisciplinary approach. Ongoing support and personalized care from a dental specialist familiar with orofacial pain and oral medicine can make a significant difference.
Concerned about burning sensations in your mouth?
Our team understands how disruptive BMS can be and is here to help with expert diagnosis and care. Contact us today to schedule a consultation.
Get In Touch
Email:
[email protected]
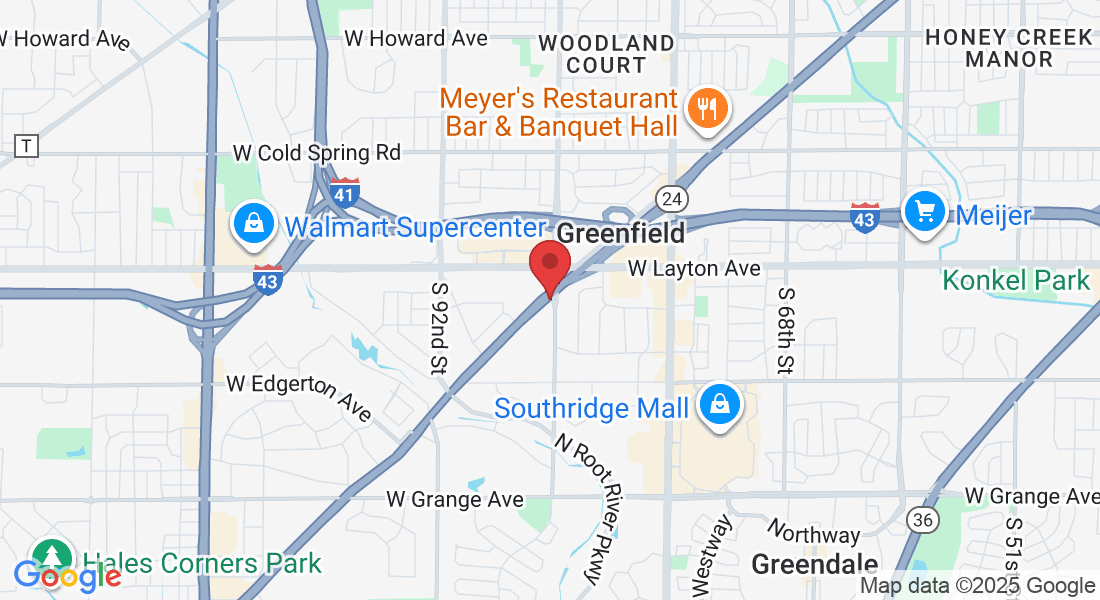
Address:
8405 W Forest Home Ave, Suite 203, Greenfield, WI 53228
Assistance Hours
Mon – Fri 8:00am – 5:00pm
Saturday/Sunday – CLOSED
Phone Number:
414-401-3144
Fax Number
414-401-3146